Epidural hematomas are severe medical conditions that demand immediate diagnosis and intervention to avoid life-threatening consequences. In this article, we discuss the causes, symptoms, and new treatment strategies for the management of epidural hematomas. Our goal is to present an extensive overview to assist patients and healthcare providers in managing this life-threatening condition effectively.
Introduction to Epidural Hematomas
An epidural hematoma is a form of traumatic brain injury that is marked by bleeding between the inner surface of the skull and the outermost layer of the dura mater, which is the protective covering of the brain. The condition usually occurs as a result of a ruptured blood vessel, which is usually caused by head trauma, resulting in the build-up of blood and pressure on the brain.
The leading cause of an epidural hematoma is a traumatic head injury, including one that results from falls, motor vehicle crashes, or sports-related blows. Skull fractures, especially of the temporal area where arteries are more susceptible to injury, are a significant risk factor. Other risk factors include the use of anticoagulant medications, alcoholism, and conditions making it easier for a person to bleed, such as hemophilia or other coagulation disorders.
Symptoms and Diagnosis
Symptoms of an epidural hematoma will depend on the severity but frequently consist of a loss of consciousness followed by a lucid interval, severe headache, dizziness, nausea, vomiting, and weakness in one side of the body. Other signs of warning might include confusion, dilation of one pupil, and seizures as it progresses.
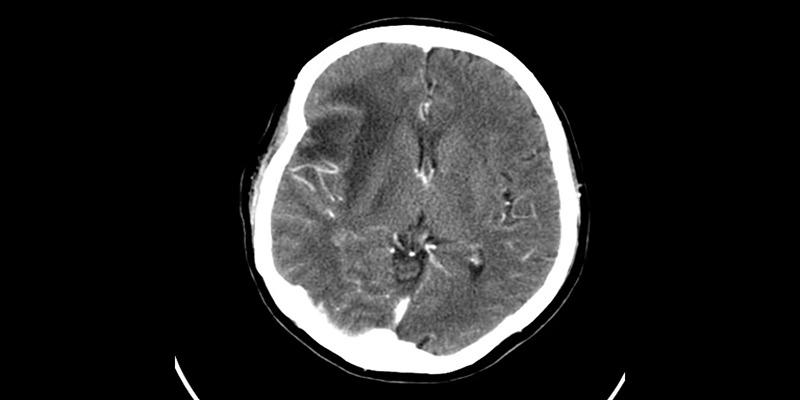
Diagnosis of an epidural hematoma usually includes imaging and diagnostic techniques like a CT scan or MRI, which determine the location, size, and pressure of the hematoma on brain structures. Proper and prompt diagnosis is essential in deciding on the treatment plan.
Surgical Treatment Options
Surgical treatment for hematomas involves various approaches, tailored to the severity, location, and underlying cause of the condition. These procedures aim to alleviate pressure on the brain and prevent long-term complications. Below are the most common surgical treatment options:
1. Craniotomy
A craniotomy is a surgical procedure where a portion of the skull is temporarily removed to directly access and remove a hematoma. It is typically performed in severe cases with extensive hemorrhaging. Once the hematoma is cleared, the skull piece is reattached. This approach helps relieve intracranial pressure and minimizes the risk of further brain damage.
2. Burr Hole Surgery
Burr hole surgery is a minimally invasive technique where small holes are drilled into the skull to drain the hematoma. It is often used for patients with subdural hematomas or cases where quick intervention is critical. The procedure is highly effective in stabilizing the patient while minimizing recovery time. However, it is generally reserved for localized bleeding.
3. Decompressive Craniectomy
Decompressive craniectomy is performed in cases of severe intracranial swelling due to hematomas. The procedure involves temporarily removing part of the skull to allow the swollen brain more room to expand without sustaining additional damage. This is often combined with other treatments to address underlying conditions.
4. Endoscopic Surgery

Endoscopic surgery is a less invasive option that uses a small camera and instruments to address the hematoma. It is particularly suitable for specialized cases, such as those involving deep-seated bleeding. Since this procedure typically requires smaller incisions, it may result in less scarring and faster recovery compared to traditional methods.
Non-Surgical Management
Non-surgical management focuses on minimizing risks and managing symptoms effectively without the need for invasive procedures. These methods are often employed when surgery is deemed unnecessary or poses added risk to the patient.
1. Medications
Medications play a critical role in managing conditions like hematomas, especially when surgery is not a viable option. Doctors often adjust anticoagulants to minimize the risk of further bleeding while still protecting against clots. Pain relievers, such as acetaminophen, are commonly prescribed to alleviate discomfort without increasing bleeding risks.
Anti-inflammatory medicines, including corticosteroids or NSAIDs, can be helpful in reducing swelling and inflammation around the affected area. In some cases, additional medications may be prescribed to address underlying health issues contributing to the condition, such as high blood pressure or anemia.
2. Compression Therapy
Compression therapy involves the use of tight bandages, wraps, or specially designed garments to apply controlled pressure to the affected area. This technique is highly effective in reducing swelling, maintaining proper blood flow, and preventing the accumulation of excess fluids. It also supports the body's natural healing process by stabilizing the area and promoting better circulation.
Compression therapy is especially beneficial in cases where hematomas are localized and manageable without surgical intervention. However, it is crucial to tailor the level of compression to each patient’s specific needs, as excessive pressure may cause discomfort or impede circulation.
3. Observation and Monitoring
For certain patients, particularly those with mild hematomas or stable symptoms, observation may be the most appropriate course of action. This non-invasive approach focuses on closely monitoring the condition to ensure it does not worsen or lead to complications.
Regular check-ups with healthcare providers are essential, often accompanied by routine imaging tests such as CT scans, MRIs, or ultrasounds to evaluate progress and detect any hidden issues. In addition, healthcare professionals may assess vital signs, such as blood pressure and heart rate, to identify any underlying concerns that could affect recovery.
4. Lifestyle Modifications
Adopting healthier lifestyle habits can significantly aid in recovery and prevent further complications from hematomas. Dietary adjustments are often recommended, such as reducing sodium intake to decrease fluid retention and incorporating nutrient-rich foods that support healing, like fruits, vegetables, and lean proteins.
Conclusion
Effective treatment of epidural hematomas hinges on prompt diagnosis and timely intervention. Whether through surgical procedures like craniotomy or less invasive methods such as observation and medication, the goal remains to relieve pressure, prevent further brain damage, and support recovery. Individualized care, combined with careful monitoring and lifestyle adjustments, can significantly improve outcomes. Early medical attention and a structured treatment approach are essential for reducing risks and ensuring the best possible prognosis for patients facing this serious condition.